History of Research on Phospholipid Metabolism and Applications to the Detection, Diagnosis, and Treatment of Cancer
Published 2022-03-07
Keywords
- Phospholipid metabolism,
- Phosphocholine,
- MRS,
- PET,
- Choline kinase
- Cancer diagnosis ...More
How to Cite
Copyright (c) 2022 Jack Cohen, Peter Daly

This work is licensed under a Creative Commons Attribution 4.0 International License.
Abstract
In the past 30 years there has been a significant increase in the number of publications on phospholipid (PL) metabolism, both for the medical purposes of detection and diagnosis of cancer and for the monitoring of the treatment of human cancers. Most of the work has focused on the pathway that produces phosphatidylcholine, the major component of human cell membranes. The trigger for this research was the advent of applications of NMR spectroscopy in vitro and in vivo in the 1980’s and observations that most cancer cells and tumors had significant increases in the water-soluble PL precursors and breakdown products. Increased phosphocholine (PC) has been focused on as a marker for cancer using Magnetic Resonance Spectroscopy (MRS) and Positron Emission Tomography (PET). MRS is now used clinically to aid in the diagnosis and severity of some brain tumors; and choline PET is used for the diagnosis and staging of recurrent prostate cancer, paid for by medical insurance companies. Another major area of research starting in the 1990’s was the development of specific choline kinase (CK) inhibitors aimed at the isoenzyme CK-a. This isoenzyme is markedly upregulated in cancer cells and unexpectedly was found to have a role in oncogenic transformation independent of its enzyme function.
References
- Théodore Gobley, Recherches chimiques sur le jaune d'œuf [Chemical researches on egg yolk], Journal de Pharmacie et de Chemie. 9 81–91, 1846.
- Théodore Gobley, Sur la lécithine et la cérébrine [On lecithin and cerebrin], Journal de Pharmacie et de Chimie 19 346–53, 1874.
- Albert L. Lehninger, Biochemistry. 2nd ed., Worth, 1970.
- William T. Evanochko, Ted T. Sakai, Thian C Ng, N. Rama Krishna, Hyun Dju Kim, Robert B. Zeidler, Vithal K. Ghanta, R. Wallace Brockman, Lewis M. Schiffer, NMR study of in vivo RIF-1 tumors. Analysis of perchloric acid extracts and identification of proton, phosphorus-31, and carbon-13 resonances, Biochim. et Biophys. Acta, Molec. Cell Res. 805 104-16, 1984.
- Britton Chance, Yuzo Nakase, Meredith Bond, John S. Jr Leigh, George McDonald, Detection of phosphorus-31 nuclear magnetic resonance signals in brain by in vivo and freeze-trapped assays, Proc. Nat. Acad. Sci. USA 75 4925-9, 1978.
- C. D'Ambrosio, B. Chance, Jr. J.S.Leigh, S. Eleff, In Vivo Phosphate Levels in Small and Large Animals, in Noninvasive Probes of Tissue Metabolism, ed. by J. S. Cohen, Wiley-Interscience, NY, pp. 209-23.1982,
- Mildred Cohn, Thomas R. Jr. Hughes, Phosphorus magnetic resonance spectra of adenosine di- and triphosphate. I. Effect of pH, J. Biol. Chem. 235, 3250-3 1960.
- D. L. Foxall, J. S. Cohen, NMR Studies of Perfused Cells, J. Mag. Res. 52 346-49, 1983.
- D. L. Foxall, J. S. Cohen, J. B. Mitchell, Continuous Perfusion of Mammalian Cells Embedded in Agarose Gel Threads Exp. Cell Res. 154 521-29, 1984.
- T. C. Ng, W. T Evanochko, J. D. Glickson, Faraday shield for surface-coil studies of subcutaneous tumors, J. Mag. Res. 49 526-9 1982.
- R. C. Lyon, P. F. Daly, J. S. Cohen, Effects of Drugs on the Metabolism of Human Cancer Cells in Vitro and Implanted in Mice Monitored by Magnetic Resonance Spectroscopy, in NMR Spectroscopy and Drug Development,, ed. by J. W. Jaroszewski, J. Schaumberg, M. Kofod, Benzon Fndtn. Symp,, Copenhagen, Vol. 26, pp. 508-29.1988,
- R. C. Lyon, R. G. Tschudin, J. S. Cohen, A Versatile Multinuclear Probe Designed for In Vivo NMR Spectroscopy: Applications to Subcutaneous Human Tumors in Mice, Mag. Res. Med. 6 1-14, 1988.
- P. F. Daly, R. C. Lyon, P. J. Faustino, J. S. Cohen, Phospholipid metabolism in cancer cells monitored by 31P NMR spectroscopy, J. Biol. Chem. 262 14875-78, 1987.
- R. C. Lyon, J. S. Cohen, P. J. Faustino, F. Megnin, C. E. Myers, Glucose Metabolism in Drug-Sensitive and Drug-Resistant Human Breast Cancer Cells Monitored by Magnetic Resonance Spectroscopy, Cancer Res. 48 870-77, 1988.
- J. Ruiz-Cabello, J.S. Cohen, Phospholipid metabolism as indicators of cancer cell function, NMR Biomed. 5 226-33,, 1992.
- P. Daly, J. S. Cohen, Magnetic Resonance Spectroscopy of Tumors and Potential in vivo Clinical Applications: a Review, Cancer Res. 49 770-79, 1989.
- Kristine Glunde, Zaver M. Bhujwalla, Sabrina M. Ronen, Choline metabolism in malignant transformation, Nature Reviews Cancer 11 835–48, 2011.
- Kristine Glunde, Marie-France Penet, Lu Jiang, Michael A Jacobs, Zaver M Bhujwalla, Choline metabolism-based molecular diagnosis of cancer: an update, Expert Rev Mol Diagn. 15 735–47, 2015.
- Franca Podo, Tumour phospholipid metabolism, NMR in Biomedicine 12 413-39, 1999.
- Gengshu Wu, Dennis E. Vance, Choline kinase and its function, Biochem. and Cell Biol. 88 559-64, 2010.
- Vladimir Sklenar, Ad Bax, A new water suppression technique for generating pure-phase spectra with equal excitation over a wide bandwidth, J. Mag Res. 75 378-83, 1987.
- P A Bottomley, Spatial localization in NMR spectroscopy in vivo, Ann. NY Acad. Sci. 508 333-48, 1987.
- P. C. M. van Zijl, C. T. W. Moonen, J. Gillen, P. F. Daly, J. F. Frank, T. F. DeLaney, O. Kaplan, J. S. Cohen, Proton magnetic resonance spectroscopy of small regions (1 mL) localized inside human tumors: a clinical feasibility study, NMR Biomed. 3 227-32, 1990.
- Jaden D. Evans, Krishan R.Jethwa, Piet Ost, Scott Williams, Eugene D.Kwon, Val J. Lowe, Brian J. Davis, Prostate cancer–specific PET radiotracers: A review on the clinical utility in recurrent disease, Practical Radiation Oncology 8 28-39, 2018.
- Michael J. Phelps, Metabolic Imaging and Positron Computed Tomography, in Noninvasive Probes of Tissue Metabolism, ed. by J. S. Cohen, Wiley-Interscience, NY, pp. 225-64.1982,
- BD. Weinberg, M. Kuruva, H. Shim, ME. Mullins, Clinical Applications of Magnetic Resonance Spectroscopy in Brain Tumors: From Diagnosis to Treatment, Radiol. Clin. North Am. 59 349-62, 2021
- Sean P. Arlauckas, Anatoliy V. Popov, E. James Delikatny, Choline kinase alpha-Putting the ChoK-hold on tumor metabolism, Progress in Lipid Research 63 28-40, 2016.
- Belén Rubio?Ruiz, Lucía Serrán?Aguilera, Ramón Hurtado?Guerrero, Ana Conejo?García, Recent advances in the design of choline kinase ? inhibitors and the molecular basis of their inhibition, Medicinal Res. Rev. 41 902-27, 2021.
- Eugene Kennedy, The function of cytidine coenzymes in the biosynthesis of phospholipides, J. Biol. Chem. 222 193 – 214, 1956.
- E. Iorio, D. Mezzanzanica, P. Alberti, F. Spadaro, C. Ramoni, S. D’Ascenzo, D. Millimaggi, A. Pavan, V. Dolo, S. Canevari, F. Podo, Alterations of choline phospholipid metabolism in ovarian tumor progression, Cancer Research 65 9369–76, 2005.
- Federica Gibellini, Terry K.Smith, The Kennedy pathway-De novo synthesis of phosphatidylethanolamine and phosphatidylcholine, IUBMB Life 62 414-28, 2010.
- Steven L. Pelech, Dennis E. Vance, Regulation of phosphatidylcholine biosynthesis, Biochim. Biophys. Acta 779 217-51, 1984.
- H. Cai, P. Erhardt, J. Troppmair, M. T. Diaz-Meco, G. Sithanandam, U. R. Rapp, J. Moscat, G. M. Cooper, Hydrolysis of phosphatidylcholine couples Ras to activation of Raf protein kinase during mitogenic signal transduction, Mol. Cell. Biol. 13 7645-51 1993.
- A. Cuadrado, A. Carnero, F. Dolfi, B. Jimenez, J. C. Lacal, Phosphorylcholine: a novel second messenger essential for mitogenic activity of growth factors, Oncogene 8 2959-68, 1993.
- J. H. Exton, Phosphatidylcholine breakdown and signal transduction, Biochim. Biophys. Acta. 1212 26-42, 1994.
- Steven L. Pelech, Dennis E. Vance, Signal transduction via phosphatidylcholine cycles, Trends Biochem. Sci. 14 28-30,, 1989.
- M. Malumbres, M. Barbacid, RAS oncogenes: the first 30 years, Nature Reviews, Cancer 3 459–65 2003.
- Eric O. Aboagye, Zaver M. Bhujwalla, Malignant Transformation Alters Membrane Choline Phospholipid Metabolism of Human Mammary Epithelial Cells, Cancer Res. 59 80-84, 1999.
- Raj K. Gupta, Jeffrey L. Benovic, Zelda B. Rose, The determination of the free magnesium level in the human red blood cell by phosphorus-31 NMR, J. Biol. Chem. 253 6172-6 1978.
- L. Jacobsen, J. S. Cohen, Improved Technique for the Investigation of Cell Metabolism, Biosci. Rep. 1 141, 1981.
- J. S. Cohen, R. C. Lyon, P. F. Daly, Monitoring Intracellular Metabolism by NMR, Methods Enzymol. 177 435-38, 1989.
- R. Knop, C.-W. Chen, J. B. Mitchell, A. Russo, S. McPherson, J. S. Cohen, Metabolic Studies of Mammalian Cells by 31P NMR Using a Continuous Perfusion Technique, Biochim. Biophys. Acta. 894 275-84, 1984.
- O. Kaplan, J. S. Cohen, Lymphocyte activation and phospholipid pathways: 31P magnetic resonance studies,, J. Biol. Chem. 265 20712-18, 1991.
- J. Ruiz-Cabello, J. S. Cohen, NMR and the study of pathological state in cells and tissues, Intl. Rev. Cytology 145 1-63, 1992.
- M. Sterin, J. Cohen, Y. Mardor, E. Berman, I. Ringel, Levels of Phospholipid Metabolites in Breast Cancer Cells Treated with Anti-mitotic Drugs: A 31P Magnetic Resonance Spectroscopy Study, Cancer Res. 61 7536-43, 2001.
- M. Sterin, J. Cohen, I. Ringel, Hormone sensitivity is reflected in the phospholipid profile in breast cancer cells, Breast Cancer Res. & Treat. 87 1-11, 2004.
- J. S. Cohen, R. C. Lyon, R. C. Chen, P. J. Faustino, G. Batist, M. Shoemaker, E. Rubalcaba, K. H. Cowan, Differences in phosphate metabolite levels in drug-sensitive and -resistant human breast cancer cell lines determined by 31P magnetic resonance spectroscopy,, Cancer Res. 46 4087-90, 1986.
- YL Ting, D Sherr, H Degani, Variations in energy and phospholipid metabolism in normal and cancer human mammary epithelial cells, Anticancer Research 16 1381-88, 1996.
- Kanchan Sonkar, Vinay Ayyappan, Caitlin M. Tressler, Oluwatobi Adelaja, Ruoqing Cai, Menglin Cheng, Kristine Glunde, Focus on the glycerophosphocholine pathway in choline phospholipid metabolism of cancer, NMR in Biomedicine 32 e4112, 2019.
- HM Baek, JH Chen, K Nie, HJ Yu, S Bahri, RS Mehta, O Nalcioglu, MY Su, Predicting pathologic response to neoadjuvant chemotherapy in breast cancer by using MR imaging and quantitative 1H MR spectroscopy, Radiology 251 653-62, 2009.
- MA. Jacobs, PB. Barker, PA. Bottomley, Z. Bhujwalla, DA. Bluemke, Proton magnetic resonance spectroscopic imaging of human breast cancer: a preliminary study, J Mag. Res. Imaging 19 68-75, 2004
- SJ Booth, MD Pickles, LW Turnbull, In vivo magnetic resonance spectroscopy of gynaecological tumours at 3.0 Tesla, BJOG 116 300-3, 2009.
- E Ackerstaff, BR Pflug, JB Nelson, ZM Bhujwalla, Detection of increased choline compounds with proton nuclear magnetic resonance spectroscopy subsequent to malignant transformation of human prostatic epithelial cells, Cancer Res. 61 3599-603, 2001.
- J Kurhanewicz, MG Swanson, SJ Nelson, DB Vigneron, Combined magnetic resonance imaging and spectroscopic imaging approach to molecular imaging of prostate cancer, J Mag. Res. Imaging 16 451-63, 2002.
- D. Belki?, K. Belki?, In vivo magnetic resonance spectroscopy for ovarian cancer diagnostics: quantification by the fast Padé transform, J. Mathematical Chem. 55 349–405, 2017.
- A Elkhaled, L Jalbert, A Constantin, HA Yoshihara, JJ Phillips, AM Molinaro, SM Chang, SJ Nelson, Characterization of metabolites in infiltrating gliomas using ex vivo ¹H high-resolution magic angle spinning spectroscopy, NMR Biomed. 27 578-9, 2014
- D Vigneron, A Bollen, M McDermott, L Wald, Day, M, S Moyher-Noworolski, R Henry, S Chang, M Berger, W Dillon, S Nelson, Three-dimensional magnetic resonance spectroscopic imaging of histologically confirmed brain tumors, Mag. Res. Imaging 19 89-101, 2001.
- S Trousil, P Lee, DJ Pinato, JK Ellis, R Dina, EO Aboagye, HC Keun, R Sharma, Alterations of choline phospholipid metabolism in endometrial cancer are caused by choline kinase alpha overexpression and a hyperactivated deacylation pathway, Cancer Res. 74 6867-77, 2014.
- P. F. Daly, Lyon, R. C., Straka, E. J., and Cohen, J. S. , 31P NMR spectroscopy of human cancer cells proliferating in a basement membrane gel, FASEB J. 2 2596-604, 1988.
- R. S. Balaban, D. G. Gadian, G. K. Radda, G. G. Wong, An NMR probe for the study of aerobic suspensions of cells and organelles, Analytical Biochemistry 116 450-5, 1981.
- A. A. De Graaf, R. M. Wittig, U. Probst, J. Strohhaecker, S. M. Schoberth, H. Sahm, Continuous-flow NMR bioreactor for in vivo studies of microbial cell suspensions with low biomass concentrations, J. Mag. Res. 98 654-9, 1992.
- Robert J. Gillies, Neil E. MacKenzie, Bruce E. Dale, Analyses of bioreactor performance by nuclear magnetic resonance spectroscopy, Bio/Technology 7 50-4, 1989.
- R. C. Lyon, P. J. Faustino, J. S. Cohen, A Perfusion Technique for 13C NMR Studies of the Metabolism of 13C-Labeled Substrates by Mammalian Cells, Mag. Res. Med 3 663-72,, 1986.
- D. L. Foxall, J. S. Cohen, R. G. Tschudin, Selective Observation of 13C Enriched Metabolites by 1H NMR, J. Mag. Res. 51 330-34, 1983.
- Y. Mardor, O. Kaplan, M. Sterin, J Ruiz Cabello, E. Ash, Y. Roth, I. Ringel, J. S. Cohen, Non-invasive real-time monitoring of intracellular cancer cell metabolism and response to lonidamine treatment using diffusion weighted proton MRS, Cancer Res. 60 5179-86, 2000.
- HM Baek, JH Chen, O Nalcioglu, MY Su, Choline as a biomarker for cell proliferation: do the results from proton MR spectroscopy show difference between HER2/neu positive and negative breast cancers?, Int J Cancer 123 1219, 2008.
- C. C. Hanstock, D. L. Rothman, T. Jue, R. G. Shulman, Volume selected proton spectroscopy in the human brain, J. Magn. Reson. 77 583-88, 1988.
- P. R. Luyten, J. A. den Hollander, C. Segebarth, D. Baleriaux, Localized 'H NMR spectroscopy and spectroscopic imaging of human brain tumors in situ, 7th Ann. Meet. Soc. Magn. Reson. Med Abstract 252, 1988.
- T. Hara, N. Kosaka, N. Shinoura, T. Kondo, PET imaging of brain tumor with [methyl-11C]choline, J. Nucl. Med. 38 842–47, 1997.
- RP. Friedland, CA. Mathis, TF. Budinger, et al., Labeled choline and phosphorylcholine: body distribution and brain autoradiography: concise communication., J. Nucl. Med. 24 812-15, 1983.
- B. Scher, M. Seitz, W. Albinger, et al., Value of 11C-choline PET and PET/CT in patients with suspected prostate cancer, Eur. J. Nucl. Med. Mol. Imaging 34 45-53, 2007.
- M. Tian, H. Zhang, N. Oriuchi, T. Higuchi, K. Endo, Comparison of 11C-choline PET and FDG PET for the differential diagnosis of malignant tumors, Eur. J. Nucl. Med. Mol. Imaging 31 1064-72, 2004.
- G. Giovacchini, E. Giovannini, R. Leoncini, et al., PET and PET/CT with radiolabeled choline in prostate cancer: a critical reappraisal of 20 years of clinical studies, Eur. J. Nucl. Med. Mol. Imaging 44 1751, 2017.
- TR. DeGrado, SW. Baldwin, Wang S, et al., Synthesis and Evaluation of 18F-Labeled Choline Analogs as Oncologic PET Tracers, J. Nucl. Med. 42 1805 – 14, 2001.
- TR. DeGrado, RE. Coleman, S. Wang, SW. Baldwin, MD. Orr, CN. Robertson, et al., Synthesis and evaluation of 18F-labeled choline as an oncologic tracer for positron emission tomography: initial findings in prostate cancer, Cancer Res. 61 110–17, 2001.
- C. Brogsitter, K. Zophel, J. Kotzerke, (18)F-choline, (11)C-choline and (11)C-acetate PET/CT: comparative analysis for imaging prostate cancer patients, Eur. J. Nucl. Med. Mol. Imaging 40 (Supp) 18–27, 2013.
- P. Mapelli, E. Incerti, F. Ceci, et al., 11C- or 18F-choline PET/CT for imaging evaluation of biochemical recurrence of prostate cancer, J. Nucl. Med. 57 43S–8S.143, 2016.
- FE. von Eyben, K. Kairemo, Acquisition with (11)C-choline and (18)F-fluorocholine PET/CT for patients with biochemical recurrence of prostate cancer: a systematic review and meta-analysis, Ann. Nucl. Med. 30 385–92, 2016.
- A. Ramirez de Molina, A. Rodriguez-Gonzalez, R. Gutierrez, L. Martinez-Pineiro, Bonilla Sanchez J, F., et al., Overexpression of choline kinase is a frequent feature in human tumor-derived cell lines and in lung, prostate, and colorectal human cancers, Biochem Biophys Res Commun. 296 580–83, 2002.
- Toshihiko Hara, 18F-Fluorocholine: A New Oncologic PET Tracer, J. Nucl. Med. 42 1815-17, 2001.
- M. Picchio, C. Messa, C. Landoni, et al., Value of [11C] choline-positron emission tomography for re-staging prostate cancer: a comparison with [18F] fluorodeoxyglucose-positron emission tomography, J. Urol. 169 1337–40, 2003.
- MD. Farwell, DA. Pryma, DA. Mankoff, PET/CT imaging in cancer: current applications and future directions, Cancer Res. 120 3433-45, 2014.
- Roger Li, Gregory C. Ravizzini, Michael A. Gorin, et al., The use of PET/CT in prostate cancer, Prostate Cancer and Prostatic Diseases 21 4–21, 2018.
- A. Roland, C. Drouet, H. Boulahdour, et al., Unusual uptakes on 18F-fluorocholine positron emission tomography/computed tomography (PET/CT): a retrospective study of 368 prostate cancer patients referred for a biochemical recurrence or an initial staging, Quant. Imaging Med. Surg. 11 172-82, 2021.
- V. Niziers, R. Boissier, D. Borchiellini, et al., "Real-world" evaluation of 18F-Choline PET/CT practices in prostate cancer patients and impact on changes in therapeutic strategy, Urol. Oncol. 38 2.e1-2.e9, 2020.
- G. Martorana, R. Schiavina, B. Corti, et al., 11C-choline positron emission tomography/computerized tomography for tumor localization of primary prostate cancer in comparison with 12-core biopsy, J. Urol. 176 954-60, 2006.
- H. Watanabe, M. Kanematsu, H. Kondo, et al., Preoperative detection of prostate cancer: a comparison with 11C-choline PET, 18F-fluorodeoxyglucose PET and MR imaging, J. Magn. Reson. Imaging 31 1151-6, 2010
- JB. Pinaquy, H. De Clermont-Galleran, G. Pasticier, et al., Comparative effectiveness of [(18) F]-fluorocholine PET-CT and pelvic MRI with diffusion-weighted imaging for staging in patients with high-risk prostate cancer, Prostate Cancer and Prostatic Diseases 75 323-31, 2015.
- L. Evangelista, F. Zattoni, A. Guttilla, et al., Choline PET or PET/CT and biochemical relapse of prostate cancer: a systematic review and meta-analysis, Clin. Nucl. Med. 38 305-14, 2013.
- N. Mottet, et al., European Association of Urology: Guidelines on Prostate Cancer, https://uroweb.org/guideline/prostate-cancer/, 2021.
- IJ. de Jong, J. Pruim, PH. Elsinga, et al., Visualization of prostate cancer with 11C-choline positron emission tomography, Eur. Urol. 42 18-23, 2002.
- R. Schiavina, V. Scattoni, P. Castellucci, et al., 11C-choline positron emission tomography/computerized tomography for preoperative lymph-node staging in intermediate-risk and high-risk prostate cancer: comparison with clinical staging nomograms, Eur. Urol. 54 392-401, 2008.
- T. Steuber, T. Schlomm, H. Heinzer, et al., [F(18)]-fluoroethylcholine combined in-line PET-CT scan for detection of lymph-node metastasis in high risk prostate cancer patients prior to radical prostatectomy: Preliminary results from a prospective histology-based study, Eur. J. Cancer 46 449-55, 2010.
- K. Kitajima, S. Yamamoto, N. Kamikonya, et al., The Potential Use of 11C-Choline Positron Emission Tomography/Computed Tomography to Monitor the Treatment Effects of Radium-223 in a Patient with Prostate Cancer, Cureus 10 e2948, 2018
- L. Evangelista, M. Cimitan, F. Zattoni, et sl., Comparison between conventional imaging (abdominal-pelvic computed tomography and bone scan) and [(18)F]choline positron emission tomography/computed tomography imaging for the initial staging of patients with intermediate- to high-risk prostate cancer: A retrospective analysis, Scand. J. Urol. 49 345-53, 2015.
- H. Kjölhede, G. Ahlgren, H. Almquist, et al., Combined 18F-fluorocholine and 18F-fluoride positron emission tomography/computed tomography imaging for staging of high-risk prostate cancer, BJU Int. 10 1501-6, 2012.
- M. Picchio, EG. Spinapolice, F. Fallanca, et al., [11C]Choline PET/CT detection of bone metastases in patients with PSA progression after primary treatment for prostate cancer: comparison with bone scintigraphy, Eur. J. Nucl. Med. Mol. Imaging 39 13-26, 2012.
- F. Bertagna, M. Abuhilal, G. Bosio, et al., Role of ¹¹C-choline positron emission tomography/computed tomography in evaluating patients affected by prostate cancer with suspected relapse due to prostate-specific antigen elevation, Jpn. J. Radiol. 29 394-404, 2011.
- K. Kitajima, RC. Murphy, MA. Nathan, et al., Detection of recurrent prostate cancer after radical prostatectomy: comparison of 11C-choline PET/CT with pelvic multiparametric MR imaging with endorectal coil, J. Nucl. Med. 55 223-32, 2014
- S. Fanti, S. Minozzi, P. Castellucci, et al., PET/CT with (11)C-choline for evaluation of prostate cancer patients with biochemical recurrence: meta-analysis and critical review of available data, Eur. J. Nucl. Med. Mol. Imaging 43 55-69, 2016
- C. Fuccio, P. Castellucci, R. Schiavina, et al., Role of 11C-choline PET/CT in the re-staging of prostate cancer patients with biochemical relapse and negative results at bone scintigraphy, Eur. J. Radiol. 81 e893-6 2012.
- C. Fuccio, P. Castellucci, R. Schiavina, et al., Role of 11C-choline PET/CT in the restaging of prostate cancer patients showing a single lesion on bone scintigraphy, Ann. Nucl. Med. 24 485-92., 2010.
- DK. Osmonov, D. Heimann, I. Janssen, et al., Sensitivity and specificity of PET/CT regarding the detection of lymph node metastases in prostate cancer recurrence, Springer Plus.??? 3 340-???, 2014.
- NM. Passoni, N. Suardi, F. Abdollah, et al., Utility of [11C]choline PET/CT in guiding lesion-targeted salvage therapies in patients with prostate cancer recurrence localized to a single lymph node at imaging: results from a pathologically validated series, Urol. Oncol. 32 e9–16, 2014.
- JA. Richter, M. Rodriguez, J. Rioja, et al., Dual tracer 11C-choline and FDG-PET in the diagnosis of biochemical prostate cancer relapse after radical treatment, Mol. Imaging Biol. 12 210–7, 2010.
- V. Scattoni, M. Picchio, N. Suardi, et al., Detection of lymph-node metastases with integrated [11C]choline PET/CT in patients with PSA failure after radical retropubic prostatectomy: results confirmed by open pelvicretroperitoneal lymphadenectomy, Eur. Urol. 52 423–9, 2007.
- D. Tilki, O. Reich, A. Graser, et al., 18F-Fluoroethylcholine PET/CT identifies lymph node metastasis in patients with prostate-specific antigen failure after radical prostatectomy but underestimates its extent. , Eur. Urol. 63 792–6, 2013.
- F. Alongi, T. Comito, E. Villa, et al., What is the role of [11C]choline PET/CT in decision making strategy before post-operative salvage radiation therapy in prostate cancer patients?, Acta Oncol. 53 990–2, 2014.
- M. Souvatzoglou, BJ. Krause, A. Purschel, et al., Influence of (11)C-choline PET/CT on the treatment planning for salvage radiation therapy in patients with biochemical recurrence of prostate cancer, Radiother. Oncol. 99 193–200, 2011.
- F. Wurschmidt, C. Petersen, A. Wahl, et al., [18F]fluoroethylcholine-PET/CT imaging for radiation treatment planning of recurrent and primary prostate cancer with dose escalation to PET/CT-positive lymph nodes, Radiat. Oncol. 6 44-??, 2011.
- HC. Rischke, W. Schultze-Seemann, G. Wieser, et al., Adjuvant radiotherapy after salvage lymph node dissection because of nodal relapse of prostate cancer versus salvage lymph node dissection only, Strahlenther Onkol. 191 310–20, 2015.
- F. Ceci, P. Castellucci, T. Graziani, et al., 11C-choline PET/CT identifies osteoblastic and osteolytic lesions in patients with metastatic prostate cancer, Clin. Nucl. Med. 40 e265–70, 2015.
- FDA approves 11C-choline for PET in prostate cancer, J. Nucl. Med. 53 11N, 2012.
- https://www.fda.gov/news-events/press-announcements/fda-approves-first-psma-targeted-pet-imaging-drug-men-prostate-cancer.
- SC. Masters, AA. Hofling, A. Gorovets, L. Marzella, FDA Approves Ga 68 PSMA-11 for Prostate Cancer Imaging, Int. J. Radiat. Oncol. Biol. Phys. 20 357-6, 2021.
- IL. Alberts, SE. Seide, C. Mingels, et al., Comparing the diagnostic performance of radiotracers in recurrent prostate cancer: a systematic review and network meta-analysis, Eur. J. Nucl. Med. Mol. Imaging Epublicaton online ahead of print. Feb 6, 2021
- C. Lawhn-Heath, A. Salavati, SC. Behr, et al., Prostate-specific Membrane Antigen PET in Prostate Cancer, Radiology 299 248-60, 2021
- MS. Hofman, N. Lawrentschuk, RJ. Francis, et al., proPSMA Study Group Collaborators. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study, Lancet 395 1208-16, 2020.
- JC. Lacal, T. Zimmerman, JM. Campos, Choline Kinase: An Unexpected Journey for a Precision Medicine Strategy in Human Diseases, Pharmaceutics 13 788-816, 2021.
- M. Cheng, ZM. Bhujwalla, K. Glunde, Targeting Phospholipid Metabolism in Cancer, Front. Oncol. 6 266-83, 2016.
- C. Aoyama, H. Liao, K. Ishidate, Structure and function of choline kinase isoforms in mammalian cells, Prog. Lipid Res. 43 266-81, 2004.
- D. Gallego-Ortega, A. Ramirez de Molina, MA. Ramos, et al., Differential role of human choline kinase alpha and beta enzymes in lipid metabolism: implications in cancer onset and treatment, PLoS One 4 e7819, 2009.
- D. Mayer, D. Werner, Inhibition of choline kinase by selectively cytotoxic purinyl-6-histamine, Biochem. Pharmacol. 23 1227-30, 1974.
- M. Hamza, J. Lloveras, G. Ribbes, et al., An in vitro study of hemicholinium-3 on phospholipid metabolism of Krebs II ascites cells, Biochem. Pharmacol. 32 1893-7, 1983.
- J. Lloveras, M. Hamza, H. Chap, L. Douste-Blazy, Action of hemicholinium-3 on phospholipid metabolism in Krebs II ascites cells, Biochem. Pharmacol. 34 3987-93, 1985.
- MV. Miceli, LS. Kan, DA. Newsome, Phosphorus-31 nuclear magnetic resonance spectroscopy of human retinoblastoma cells: correlation with metabolic indices, Biochim. Biophys. Acta 970 262-9, 1988.
- GK. Radda, RD. Oberhaensli, DJ. Taylor, The biochemistry of human diseases as studied by 31P NMR in man and animal models, Ann. NY Acad. Sci. 508 300-8, 1987.
- JC. Lacal, Choline kinase: a novel target for antitumor drugs, Drugs 4 419–26, 2001.
- A. Ramírez de Molina, D. Gallego-Ortega, J. Sarmentero, et al., Choline kinase is a novel oncogene that potentiates RhoA-induced carcinogenesis, Cancer Res. 65 5647-53, 2005.
- A. Carnero, JC. Lacal, Activation of intracellular kinases in Xenopus oocytes by p21ras and phospholipases: a comparative study, Mol. Cell Biol. 15 1094-101, 1995.
- R. Hernández-Alcoceba, L. Saniger, J. Campos, et al., Choline kinase inhibitors as a novel approach for antiproliferative drug design, Oncogene 15 2289-301, 1997.
- B. Jiménez, L. del Peso, S. Montaner, et al., Generation of phosphorylcholine as an essential event in the activation of Raf-1 and MAP-kinases in growth factors-induced mitogenic stimulation, J. Cell Biochem. 57 141-9, 1995.
- JC. Lacal, Diacylglycerol production in Xenopus laevis oocytes after microinjection of p21ras proteins is a consequence of activation of phosphatidylcholine metabolism, Mol. Cell Biol. 10 333-40, 1990.
- JC. Lacal, J. Moscat, SA. Aaronson, Novel source of 1,2-diacylglycerol elevated in cells transformed by Ha-ras oncogene, Nature Reviews Cancer 330 269-72, 1987.
- IG. Macara, Elevated phosphocholine concentration in ras-transformed NIH 3T3 cells arises from increased choline kinase activity, not from phosphatidylcholine breakdown, Mol. Cell Biol. 9 325-8, 1989.
- D. Teegarden, EJ. Taparowsky, C. Kent, Altered phosphatidylcholine metabolism in C3H10T1/2 cells transfected with the Harvey-ras oncogene, J. Biol. Chem. 265 6042-7, 1990.
- GB. Ansell, SG. Spanner, The inhibition of brain choline kinase by hemicholinium-3, J. Neurochem. 22 1153-5, 1974
- JG. Cannon, Structure-activity aspects of hemicholinium-3 (HC-3) and its analogs and congeners, Med. Res. Rev. 14 505-31, 1994
- R. Hernández-Alcoceba, F. Fernández, JC. Lacal, In vivo antitumor activity of choline kinase inhibitors: a novel target for anticancer drug discovery, Cancer Res. 59 3112-8, 1999.
- NM. Al-Saffar, H. Troy, A. Ramírez de Molina, et al., Noninvasive magnetic resonance spectroscopic pharmacodynamic markers of the choline kinase inhibitor MN58b in human carcinoma models, Cancer Res. 66 427-34, 2006.
- M. Kumar, SP. Arlauckas, S. Saksena, et al., Magnetic resonance spectroscopy for detection of choline kinase inhibition in the treatment of brain tumors, Mol. Cancer Ther. 14 899-908, 2015.
- R. Sánchez-Martín, JM. Campos, A. Conejo-García, et al., Symmetrical bis-quinolinium compounds: new human choline kinase inhibitors with antiproliferative activity against the HT-29 cell line, J. Med. Chem. 48 3354-63, 2005
- Study of Intravenous TCD-717 in Patients With Advanced Solid Tumors, Phase I trial of TCD-717, https://.gov/ct2/show/NCT01215864.
- JC. Lacal, JM. Campos, Preclinical characterization of RSM-932A, a novel anticancer drug targeting the human choline kinase alpha, an enzyme involved in increased lipid metabolism of cancer cells, Mol. Cancer Ther. 14 31-9, 2015.
- SL. Kall, EJ. Delikatny, A. Lavie, Identification of a Unique Inhibitor-Binding Site on Choline Kinase ?, Biochemistry 57 1316-25, 2018.
- SC. Falcon, CS. Hudson, Y. Huang, et al., A non-catalytic role of choline kinase alpha is important in promoting cancer cell survival, Oncogenesis 2 e38, 2013.
- N. Mori, F. Wildes, S. Kakkad, et al., Choline kinase-? protein and phosphatidylcholine but not phosphocholine are required for breast cancer cell survival, NMR Biomed. 28 1697-706, 2015.
- DI. Hoult, SJ. Busby, DG. Gadian, GK. Radda, RE. Richards, PJ. Seeley, Observation of tissue metabolites using 31P nuclear magnetic resonance, Nature Reviews Cancer 252 285-7, 1974.
- PC. Lauterbur, Image Formation by Induced Local Interactions: Examples Employing Nuclear Magnetic Resonance, Nature Reviews Cancer 242 190–91, 1973.
- ID. Cresshull, RE. Gordon, PE. Hanley, et al., Localisation of Metabolites in Animal and Human Tissues Using 31P Topical Magnetic Resonance, Bull. Magn. Res. 2 426, 1980.
- JR. Griffiths, E. Cady, RH. Edwards, et al., 31P-NMR studies of a human tumour in situ, Lancet 1 1435-6, 1983.
- JM. Maris, AE. Evans, AC. McLaughlin, et al., 31P nuclear magnetic resonance spectroscopic investigation of human neuroblastoma in situ, New Engl. J. Med. 312 1500-5, 1985
- H. Bruhn, J. Frahm, ML. Gyngell, et al., Noninvasive differentiation of tumors with use of localized H-1 MR spectroscopy in vivo: initial experience in patients with cerebral tumors, Radiology 172 541-8, 1989.
- AA. Maudsley, OC. Andronesi, PB. Barker, et al., Advanced magnetic resonance spectroscopic neuroimaging: Experts' consensus recommendations, NMR Biomed. 34 1-22, 2021.
- AC. Westphalen, Lost in translation: lessons learned from the "demise" of MRSI of the prostate, Abdom. Radiol. (NY) 44 3185-87, 2019.
- R. Faghihi, B. Zeinali-Rafsanjani, MA. Mosleh-Shirazi, et al., Magnetic Resonance Spectroscopy and its Clinical Applications: A Review, J. Med. Imaging Radiat. Sci. 48 233-53, 2017.
- https://clinicaltrials.gov/.
- PA. Bottomley, WA. Edelstein, TH. Foster, WA. Adams, In vivo solvent-suppressed localized hydrogen nuclear magnetic resonance spectroscopy: a window to metabolism?, Proc. Natl. Acad. Sci. USA 82 2148-52, 1985.
- J. Frahm, Localized Proton Spectroscopy using stimulated echoes, J. Magn. Reson. 72 502– 08, 1987.
- J. Frahm, H. Bruhn, ML. Gyngell, et al., Localized high-resolution proton NMR spectroscopy using stimulated echoes: initial applications to human brain in vivo, Magn. Reson. Med. 79-93, 1989.
- PR. Luyten, AJ. Marien, W. Heindel, et al., Metabolic imaging of patients with intracranial tumors: H-1 MR spectroscopic imaging and PET, Radiology 176 791-9, 1990.
- C. Choi, SK. Ganji, RJ. DeBerardinis, et al., 2-hydroxyglutarate detection by magnetic resonance spectroscopy in IDH-mutated patients with gliomas, Nature Med. 18 624-9, 2012.
- JH. Langkowski, J. Wieland, H. Bomsdorf, et al., Pre-operative localized in vivo proton spectroscopy in cerebral tumors at 4.0 Tesla--first results, Magn. Reson. Imaging 7 547-55, 1989.
- R. Hourani, A. Horská, S. Albayram, et al., Proton magnetic resonance spectroscopic imaging to differentiate between nonneoplastic lesions and brain tumors in children, J. Magn. Reson. Imaging 23 99-107, 2006
- P.B. Barker, N-Acetyl Aspartate—A Neuronal Marker?, Ann. Neurol. 49 423-24., 2001.
- TR. Brown, BM. Kincaid, K. Ugurbil, NMR chemical shift imaging in three dimensions, Proc. Natl. Acad. Sci. USA 79 3523-6, 1982
- Jack S. Cohen, Jerzy W. Jaroszewski, Ofer Kaplan, Jesus Ruiz-Cabello, Steven W. Collier, A history of biological applications of NMR spectroscopy, Progress Nucl. Magn. Reson. Spect. 28 53-85, 1995.
- J. Zhong, V. Huang, SS. Gurbani, et al., 3D whole-brain metabolite imaging to improve characterization of low-to-intermediate grade gliomas, J. Neurooncol. 153 303-11, 2021.
- W. Negendank, Studies of human tumors by MRS: a review, NMR Biomed. 5 303-24, 1992.
- FA. Howe, SJ. Barton, SA. Cudlip, et al., Metabolic profiles of human brain tumors using quantitative in vivo 1H magnetic resonance spectroscopy, Magn. Reson. Med. 49 223-32, 2003
- JS. Taylor, JW. Langston, WE. Reddick, t al., Clinical value of proton magnetic resonance spectroscopy for differentiating recurrent or residual brain tumor from delayed cerebral necrosis, Int. J. Radiat. Oncol. Biol. Phys. 36 1251-61, 1996.
- MC. Preul, Z. Caramanos, DL. Collins, et al., Accurate, noninvasive diagnosis of human brain tumors by using proton magnetic resonance spectroscopy, Nature Med. 2 323-5, 1996.
- MC. Preul, Z. Caramanos, R. Leblanc, et al., Using pattern analysis of in vivo proton MRSI data to improve the diagnosis and surgical management of patients with brain tumors, NMR Biomed. 11 192-200, 1998.
- FS. De Edelenyi, C. Rubin, F. Estève, et al., A new approach for analyzing proton magnetic resonance spectroscopic images of brain tumors: nosologic images, Nature Med. 6 1287-9, 2000.
- AR. Tate, JR. Griffiths, I. Martínez-Pérez, et al., Towards a method for automated classification of 1H MRS spectra from brain tumours, NMR Biomed. 11 177-91, 1998.
- AR. Tate, C. Majós, A. Moreno, et al., Automated classification of short echo time in in vivo 1H brain tumor spectra: a multicenter study, Magn. Reson. Med. 49 29-36, 2003.
- M. Julià-Sapé, JR. Griffiths, AR. Tate, et al., Classification of brain tumours from MR spectra: the INTERPRET collaboration and its outcomes, NMR Biomed. 28 1772-87, 2015.
- AR. Tate, J. Underwood, DM. Acosta, et al., Development of a decision support system for diagnosis and grading of brain tumours using in vivo magnetic resonance single voxel spectra, NMR Biomed. 19 411-34, 2006.
- A. Horská, PB. Barker, Imaging of brain tumors: MR spectroscopy and metabolic imaging, Neuroimaging Clin. N. Am. 20 293-310, 2010.
- http://www.aetna.com/cpb/medical/data/200_299/0202.html.
- https://www.uhcprovider.com/content/dam/provider/docs/public/policies/signaturevalue-mmg/magnetic-resonance-spectroscopy-sv.pdf.
- AM. Omuro, CC. Leite, K. Mokhtari, JY. Delattre, Pitfalls in the diagnosis of brain tumours, Lancet Neurol. 5 937-48, 2006.
- R. Hourani, LJ. Brant, T. Rizk, et al., Can proton MR spectroscopic and perfusion imaging differentiate between neoplastic and nonneoplastic brain lesions in adults?, Am. J. Neuroradiol. 29 366-72, 2008.
- WB. Pope, Brain metastases: neuroimaging, Handbk. Clin. Neurol. 149 89-112, 2018.
- H. Ishimaru, M. Morikawa, S. Iwanaga, et al., Differentiation between high-grade glioma and metastatic brain tumor using single-voxel proton MR spectroscopy, Eur. Radiol. 11 1784-91, 2001.
- IC. Chiang, YT. Kuo, CY. Lu, et al., Distinction between high-grade gliomas and solitary metastases using peritumoral 3-T magnetic resonance spectroscopy, diffusion, and perfusion imagings, Neuroradiology 46 619-27, 2004.
- S. Chawla, Y. Zhang, S. Wang, et al., Proton magnetic resonance spectroscopy in differentiating glioblastomas from primary cerebral lymphomas and brain metastases, J. Comput. Assist. Tomogr. 34 836-41, 2010.
- G. Fan, B. Sun, Z. Wu, Q. Guo, Y. Guo, In vivo single-voxel proton MR spectroscopy in the differentiation of high-grade gliomas and solitary metastases, Clin Radiol. 59 77-85, 2004
- A. Server, R. Josefsen, B. Kulle, et al., Proton magnetic resonance spectroscopy in the distinction of high-grade cerebral gliomas from single metastatic brain tumors, Acta Radiol. 316-25, 2010.
- LA. Brandao, M. Castillo, Lymphomas-Part 1, Neuroimaging Clin. N. Am. 26 511–36, 201 .
- H. Nagashima, T. Sasayama, K. Tanaka, et al., Myo-inositol concentration in MR spectroscopy for differentiating high grade glioma from primary central nervous system lymphoma, J. Neurooncol. 136 317–26, 2018. .
- A. Vallee, C. Guillevin, M. Wager, et al., Added Value of Spectroscopy to Perfusion MRI in the Differential Diagnostic Performance of Common Malignant Brain Tumors, Am. J. Neuroradiol. 39 1423–31, 2018.
- SS. Lu, SJ. Kim, HS. Kim, et al., Utility of proton MR spectroscopy for differentiating typical and atypical primary central nervous system lymphomas from tumefactive demyelinating lesions, Am. J. Neuroradiol. 35 270–77, 2014.
- R Ikeguchi, Y Shimizu, K Abe, et al., Proton magnetic resonance spectroscopy differentiates tumefactive demyelinating lesions from gliomas, Mult. Scler. Relat. Disord. 26 77–84, 2018.
- M. Garg, RK. Gupta, MR Spectroscopy in intracranial infection, in Clinical MR Neuroimaging: Diffusion, Perfusion and Spectroscopy, ed. by J. Gillard, A. Waldman, P. Barker, Cambridge University Press, Cambridge, UK:, pp. 380–406, 2004.
- C. Remy, S. Grand, ES. Lai, et al., 1H MRS of human brain abscesses in vivo and in vitro, Magn. Reson. Med. 34 508–14, 1995.
- D. Pal, A. Bhattacharyya, M. Husain, et al., In vivo proton MR spectroscopy evaluation of pyogenic brain abscesses: a report of 194 cases, Am. J. Neuroradiol. 31 360–66, 2010.
- O. Speck, T. Thiel, J. Hennig, Grading and therapy monitoring of astrocytomas with 1H-spectroscopy: preliminary study, Anticancer Res. 16 1581-5, 1996
- MC. Preul, R. Leblanc, Z. Caramanos, et al., Magnetic resonance spectroscopy guided brain tumor resection: differentiation between recurrent glioma and radiation change in two diagnostically difficult cases, Can. J. Neurol. Sci. 13-22, 1998.
- PE. Ricci, A. Pitt, PJ. Keller, et al., Effect of voxel position on single-voxel MR spectroscopy findings, Am. J. Neuroradiol. 21 367-74., 2000.
- C. Senft, E. Hattingen, U. Pilatus, et al., Diagnostic value of proton magnetic resonance spectroscopy in the noninvasive grading of solid gliomas: comparison of maximum and mean choline values, Neurosurgery 908-13, 2009.
- S. Chawla, S. Wang, RL. Wolf, et al., Arterial spin-labeling and MR spectroscopy in the differentiation of gliomas, Am J Neuroradiol 1683–89, 2007.
- M. Bulik, R. Jancalek, J. Vanicek, et al., Potential of MR spectroscopy for assessment of glioma grading, Clin. Neurol. Neurosurg. 115 146–53, 2013.
- Q. Wang, H. Zhang, J. Zhang, et al., The diagnostic performance of magnetic resonance spectroscopy in differentiating high-from low-grade gliomas: A systematic review and meta-analysis, Eur Radiol. 26 2670–84, 2016.
- A. Arslanoglu, D. Bonekamp, PB. Barker, et al., Quantitative proton MR spectroscopic imaging of the mesial temporal lobe, J. Magn. Reson. Imaging 20 772–78, 2004.
- AA. Chan, A. Lau, A. Pirzkall, et al., Proton magnetic resonance spectroscopy imaging in the evaluation of patients undergoing gamma knife surgery for Grade IV glioma, J. Neurosurg. 101 467–75, 2004.
- FW. Crawford, IS. Khayal, C. McGue, et al., Relationship of pre-surgery metabolic and physiological MR imaging parameters to survival for patients with untreated GBM, J. Neurooncol. 91 337–51, 2009.
- S. Saraswathy, FW. Crawford, KR. Lamborn, et al., Evaluation of MR markers that predict survival in patients with newly diagnosed GBM prior to adjuvant therapy, J. Neurooncol. 91 69–81, 2009.
- KE Warren, JA Frank, JL Black, et al., Proton magnetic resonance spectroscopic imaging in children with recurrent primary brain tumors, J. Clin. Oncol. 18 1020–26, 2000.
- K. Parvez, A. Parvez, G. Zadeh, The diagnosis and treatment of pseudoprogression, radiation necrosis and brain tumor recurrence, Int. J. Mol. Sci. 15 11832–46, 2014.
- A. Siu, JJ. Wind, JB. Iorgulescu, et al., Radiation necrosis following treatment of high grade glioma--a review of the literature and current understanding, Acta Neurochir. (Wien) 154 191–201, 2012.
- M. Chernov, M. Hayashi, M. Izawa, et al., Differentiation of the radiation-induced necrosis and tumor recurrence after gamma knife radiosurgery for brain metastases: importance of multi-voxel proton MRS, Minim. Invasive Neurosurg. 48 228-34, 2005.
- MF. Chernov, M. Hayashi, M. Izawa, et al., Multivoxel proton MRS for differentiation of radiation-induced necrosis and tumor recurrence after gamma knife radiosurgery for brain metastases, Brain Tumor Pathol. 23 19–27, 2006.
- LL. Wald, SJ. Nelson, MR. Day, et al., Serial proton magnetic resonance spectroscopy imaging of glioblastoma multiforme after brachytherapy, J. Neurosurg. 87 525–34, 1997.
- EA. Smith, RC. Carlos, LR. Junck, et al., Developing a clinical decision model: MR spectroscopy to differentiate between recurrent tumor and radiation change in patients with new contrast-enhancing lesions, Am. J. Roentgenol. 192 W45–W52, 2009.
- X. Li, DB. Vigneron, S. Cha, et al., Relationship of MR-derived lactate, mobile lipids, and relative blood volume for gliomas in vivo, Am. J. Neuroradiol. 26 760–69, 2005.
- JP. Rock, D. Hearshen, L. Scarpace, et al., Correlations between magnetic resonance spectroscopy and image-guided histopathology, with special attention to radiation necrosis, Neurosurgery 51 912–19, 2002.
- T. Nakajima, T. Kumabe, M. Kanamori, et al., Differential diagnosis between radiation necrosis and glioma progression using sequential proton magnetic resonance spectroscopy and methionine positron emission tomography, Neurol. Med. Chir. (Tokyo) 49 394–401, 2009.
- H. Zhang, L. Ma, Q. Wang, et al., Role of magnetic resonance spectroscopy for the differentiation of recurrent glioma from radiation necrosis: a systematic review and meta-analysis, Eur. J. Radiol. 83 2181–89, 2014.
- BRJ. van Dijken, PJ. van Laar, GA. Holtman , A. van der Hoorn, Diagnostic accuracy of magnetic resonance imaging techniques for treatment response evaluation in patients with high-grade glioma, a systematic review and meta-analysis, Eur. Radiol. 27 4129–44, 2017.
- A. Di Costanzo, T. Scarabino, F. Trojsi, et al., Multiparametric 3T MR approach to the assessment of cerebral gliomas: tumor extent and malignancy, Neuroradiology 48 622–31, 2006.
- EJ. Hermann, E. Hattingen, JK. Krauss, et al., Stereotactic biopsy in gliomas guided by 3-tesla 1H–chemical-shift imaging of choline, Stereotact. Funct. Neurosurg. 86 300–7, 2008.
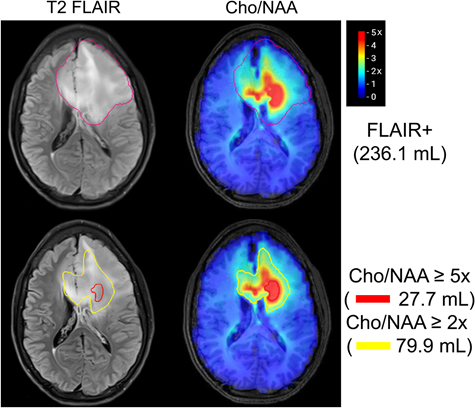
- JS. Cordova, HK. Shu, Z. Liang, et al., Whole-brain spectroscopic MRI biomarkers identify infiltrating margins in glioblastoma patients, Neuro. Oncol. 18 1180–89, 2016.
- JS. Cordova, S. Kandula, S. Gurbani, et al., Simulating the Effect of Spectroscopic MRI as a Metric for Radiation Therapy Planning in Patients with Glioblastoma, Tomography 2 366–73, 2016.
- S. Ken, L. Vieillevigne, X. Franceries, et al., Integration method of 3D MR spectroscopy into treatment planning system for glioblastoma IMRT dose painting with integrated simultaneous boost, Radiat. Oncol. 8 1, 2013.
- https://clinicaltrials.gov/ct2/show/NCT03137888
- George Shu Hui-Kuo, Eric Albert Mellon, Lawrence Kleinberg, et al., A multisite clinical trial of spectroscopic MRI-guided radiation dose escalation for newly-diagnosed glioblastomas, J. Clin.Oncol. 39:15 suppl 2018, 2021.
- M Wilson, O Andronesi, PB Barker, et al.. Methodological consensus on clinical proton MRS of the brain: Review and recommendations., Magn. Reson. Med. 82 527-50, 2019.
- https://www.gehealthcare.com/article/15t-compared-to-30t-mri-scanners.
- A. Nowogrodzki, The world's strongest MRI machines are pushing human imaging to new limits, Nature Med. 563 24-26, 2018.
- M.A. Thomas, P. Narayan, J. Kurhanewicz, et al., 1H MR spectroscopy of normal and malignant human prostates in Vivo, , Journal of Magnetic Resonance 87 610-19, 1990.
- J. Kurhanewicz, A. Thomas, P. Jajodia, et al., 31P spectroscopy of the human prostate gland in vivo using a transrectal probe., Magn. Reson. Med. 22 404-13, 1991
- J. Kurhanewicz, DB. Vigneron, H. Hricak, et al., Three-dimensional H-1 MR spectroscopic imaging of the in situ human prostate with high (0.24-0.7-cm3) spatial resolution, Radiology 198 795-805, 1996.
- JO. Barentsz, J. Richenberg, R. Clements, et al., European Society of Urogenital Radiology. ESUR prostate MR guidelines 2012, Eur. Radiol. 22 746-57, 2012.
- A. Stabile, F. Giganti, AB. Rosenkrantz, et al., Multiparametric MRI for prostate cancer diagnosis: current status and future directions, Nat. Rev. Urol. 17 41-61, 2020
- F. Giganti, AB. Rosenkrantz, G. Villeirs, et al., The Evolution of MRI of the Prostate: The Past, the Present, and the Future, Am. J. Roentgenol. 213 384-96, 2019
- PE. Sijens, HK. Wijrdeman, MA. Moerland, et al., Human breast cancer in vivo: H-1 and P-31 MR spectroscopy at 1.5 T, Radiology 169 615-20, 1988.
- J. Glaholm, M. O. Leach, D. J. Collins, et al., In-vivo 31P magnetic resonance spectroscopy for monitoring tumour response in breast cancer, Lancet 333 1326–27 1989.
- T. C. Ng, S. Grundfest, S. Vijayakumar, et al., Therapeutic response of breast carcinoma monitored by 31P MRS in situ, Magn. Reson. Med. 10 125–34, 1989.
- MO. Leach, M. Verrill, J. Glaholm, et al., Measurements of human breast cancer using magnetic resonance spectroscopy: a review of clinical measurements and a report of localized 31P measurements of response to treatment, NMR Biomed. 11 314-40, 1998.
- T. A. Smith, J. Glaholm, M. O. Leach, et al., A comparison of in vivo and in vitro 31P NMR spectra from human breast tumours: variations in phospholipid metabolism, Br. J. Cancer 63 514–16, 1991.
- R. Katz-Brull, PT. Lavin, RE. Lenkinski, Clinical utility of proton magnetic resonance spectroscopy in characterizing breast lesions, J. Natl. Cancer Inst. 94 1197-203, 2002.
- GL Menezes, FM. Knuttel, BL. Stehouwer, et al., Magnetic resonance imaging in breast cancer: A literature review and future perspectives, World J. Clin. Oncol. 10 61-70, 2014.
- R. Fardanesh, MA. Marino, D. Avendano, et al., Proton MR spectroscopy in the breast: Technical innovations and clinical applications, J. Magn. Reson. Imaging 50 1033-46, 2019
- T. Shah, B. Krishnamachary, F. Wildes, et al., Molecular causes of elevated phosphoethanolamine in breast and pancreatic cancer cells, NMR Biomed. 31 e3936, 2018.
- AGV. Bitencourt, J. Goldberg, K. Pinker, SB. Thakur, Clinical applications of breast cancer metabolomics using high-resolution magic angle spinning proton magnetic resonance spectroscopy (HRMAS 1H MRS): systematic scoping review, Metabolomics 15 148, 2019.
- LA. Vandergrift, EA. Decelle, J. Kurth, et al., Metabolomic Prediction of Human Prostate Cancer Aggressiveness: Magnetic Resonance Spectroscopy of Histologically Benign Tissue, Sci. Rep. 8 4997, 2018.
- M. Donadon, E. Lopci, J. Galvanin, et al., Prognostic Value of Metabolic Imaging Data of 11C-choline PET/CT in Patients Undergoing Hepatectomy for Hepatocellular Carcinoma, Cancers 13 472, 2021.
- G. Treglia, A. Piccardo, A. Imperiale, et al., Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis, Eur. J. Nucl. Med. Mol. Imaging 46 751-65, 2019.




